SLAP Injury
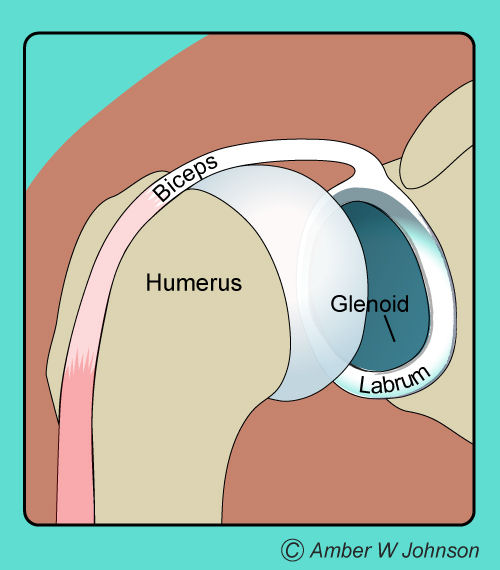
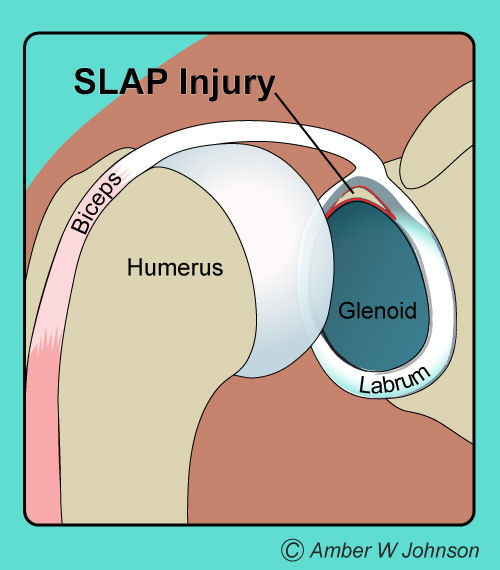
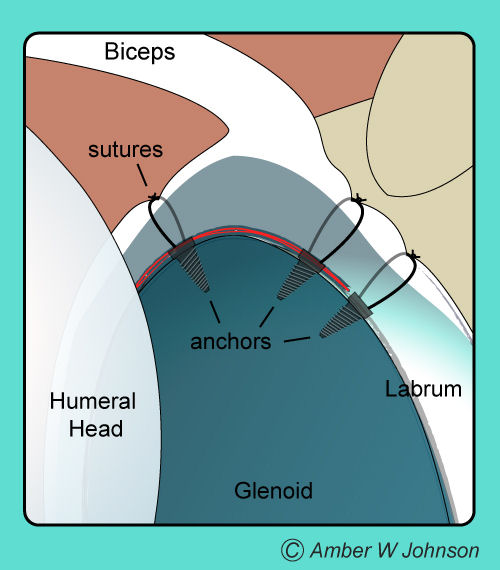
The shoulder joint is like a ball and socket. The socket is like a shallow cup with a meniscus or rope-like rim called the labrum. The top of the labrum acts as a biceps tendon attachment and this is the area where SLAP tears occur. Tears can occur at any portion of the labrum.

What is a SLAP Injury?
Labral tears of the superior labrum have been recognized for many years. Andrews first recognized Superior Labral Tears in throwing athletes in 1985. Later in 1990, Snyder classified these lesions and coined the term “SLAP” for Superior Labrum Anterior Posterior lesions.
Type I is a frayed labrum but still attached to the glenoid rim superiorly.
Type II have detached labrum from the rim with detached biceps anchor.
Type III are described as “bucket handle” like, the labrum is torn away yet the biceps anchor remains.
Type IV are a bucket handle tear with a tear that extends into the biceps.
Symptoms and Diagnosis:
History is important since SLAP tears are felt to occur from repetitive trauma in overhead throwers such as baseball players, volleyball players, basketball players. SLAP tears can also occur from climbing accidents, climbing injuries, falls, and/or lifting heavy objects acutely.
Symptoms are often vague and difficult to interpret. There is often a deep ache, clicking or grinding with motion of the shoulder. A throwing position may make symptoms worse and often there is moderate difficulty in sleeping on that shoulder at nights.
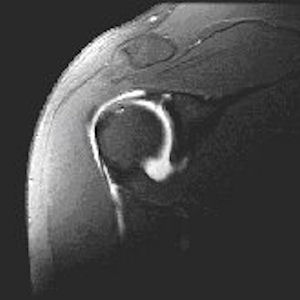
Diagnosis can be difficult but usually can be made with a good physical exam. X-rays are often taken to rule out small fractures of the rim of the glenoid or bone spurs, and a MRI arthrogram, which is an MRI with a dye injection into the shoulder, is often helpful to confirm the diagnosis. It may also help rule out other causes of pain such as a rotator cuff tear or biceps tear. MRIs are not always required, however occasionally a coexistent rotator cuff tear may exist. SLAP tears may lead to early arthritis of the shoulder joint by wear and tear of the flap or labrum rim in the joint.
Treatment Options:
Usually depends on activity level and symptoms. Often ice, heat, anti-inflammatories, as well as physical therapy are tried for a period of time. If conservative treatment fails with persistence of symptoms, then arthroscopic evaluation and treatment is considered.
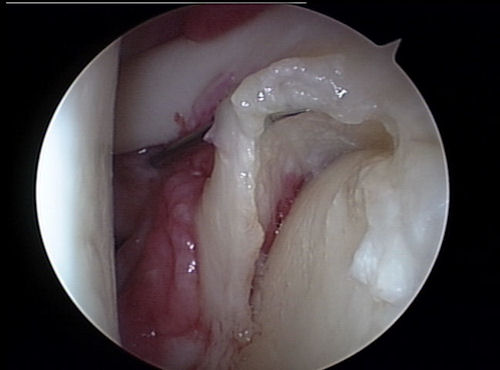
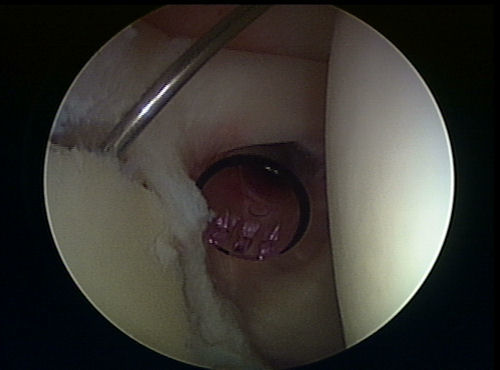
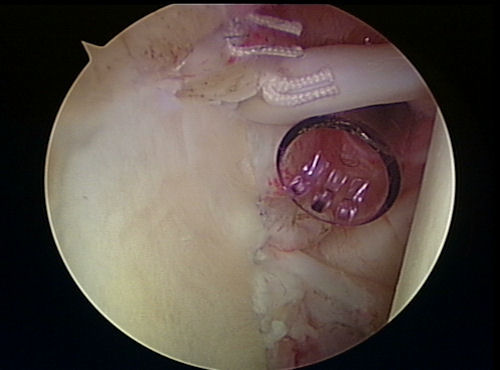
SLAP tears are usually repaired with an arthroscopic means if the repair or debridement is possible. For either, a small 3- to 5-mm diameter arthroscope is inserted into either the front, lateral, anterior or all three positions for the shoulder diagnosis and for confirmation of the injury.
Next, the tear is debrided (another word for trimmed) and/or repaired. The repair requires roughening of the rim of the glenoid superiorly and then placement of small suture anchors into the bone with the sutures tied over the labrum and/or biceps anchor for repair.
If the SLAP is found to be un-repairable, because of its poor tissue or nature and extent of tear, then the biceps tenodesis is performed. Biceps tenodesis is a procedure where the biceps insertion at the top of the labrum is actually cut, through the scope, and then either through arthroscope or small anterior open incision the biceps is inserted into the bone of the bicipital groove within the neck of the humerus. This procedure is often performed in patients that are over 40 years of age or with a type IV lesion, or if there is a moderate degenerative tear that has been present for a long time and does not have a high likelihood of healing with repair.
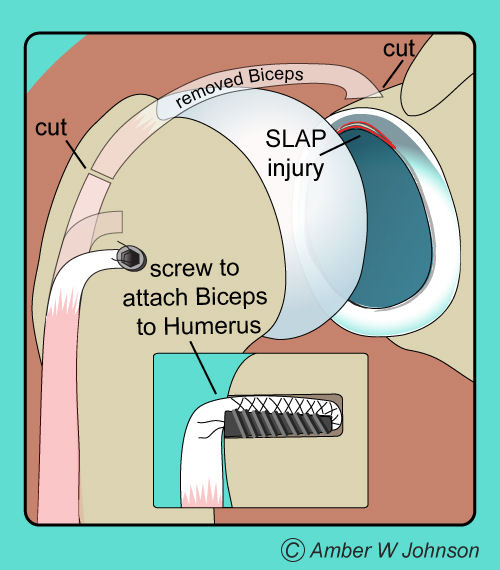
Bicep tenodesis
Post Operative Rehabilitation:
SLAP Repair Protocol:
SLAP Debridement + Bicep Tenotomy:
Note: These instructions are to serve as guidelines and are subject to Physician discretion. Actual results may be faster or slower depending on the individual.


